Neuroscience
The Second Brain in Our Gut
There are more than 100 million neurons in our gut. That is why it is also known as the second brain. Researchers from Bochum are uncovering the role of the brain-gut connection in learning and unlearning pain.
Butterflies in your tummy, nervous stomach rumblings, hunger: Our brain and gut are in constant communication with each other. This communication is particularly intense when we experience pain arising from the gastrointestinal tract. When fear of such pain becomes worse than the pain itself, this is often the result of learning processes. Professor Adriane Icenhour and Dr. Franziska Labrenz from Collaborative Research Center 1280 are investigating how people could be helped to overcome the vicious circle of fear and pain.
Professor Icenhour, what does pain have to do with learning processes?
Adriane Icenhour: We are all familiar with this: When we are in pain, we start to worry and wonder what is wrong and what we can do about it. Go to the doctor? Take a tablet? Rest and regenerate? Pain is one of the most important warning signals and a high motivation for the body – and therefore particularly powerful to stimulate learning processes so that we can adapt to the unpleasant situation or, more importantly, avoid experiencing it again in the future. What can we do to prevent pain from arising in the first place? Which signals from outside or inside the body should we regard as warning signals in the future so that the pain will not occur at all?
In your research projects, you are looking at a very specific type of pain, visceral pain. What characterizes it?
Icenhour: Visceral pain can be translated as pain arising from our internal organs and encompasses all aversive sensations from our gastrointestinal tract, from painful belching to abdominal pain. This type of pain from the inside of our body is special in that it is perceived as much more frightening than pain from the outside of the body. We can’t escape it – not in the same way that we quickly pull our hand away from a hot hob, for example. And: We are often unable to say exactly what hurts. We have a diffuse discomfort that is difficult to localize and we are unable to do anything about it.
The term “brain-gut axis” is often used in this context. What does this mean?
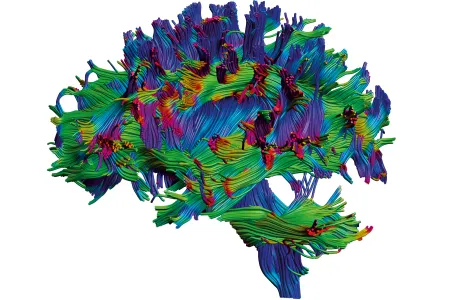
Icenhour: Wetting your pants from anxiety or stress that upsets your stomach: In our everyday language, the connection between the brain and the gastrointestinal tract is intuitively understandable. It has been scientifically shown that signals from inside the body are communicated along the brain-gut axis via various messenger substances. And this happens constantly and often unnoticed. This communication is bidirectional: Our brain, including our emotions, influences gastrointestinal processes and vice versa.

You can hardly distinguish between the cluster of nerves in the gut and that in the brain.
Franziska Labrenz: Our intestines are not just one organ, but one of three nervous systems. In addition to our central and peripheral nervous system, there is also the so-called enteric nervous system, which runs through our gastrointestinal tract. Just as we have nerve cells in our brain, we also have nerve cells in our intestines – around 100 million of them. And this second brain has a very similar structure. You can hardly distinguish between the cluster of nerves in the gut and that in the brain.

In your research projects, you are trying to find out how visceral pain is communicated along this axis, how it is learned and unlearned. What do the learning experiments look like?
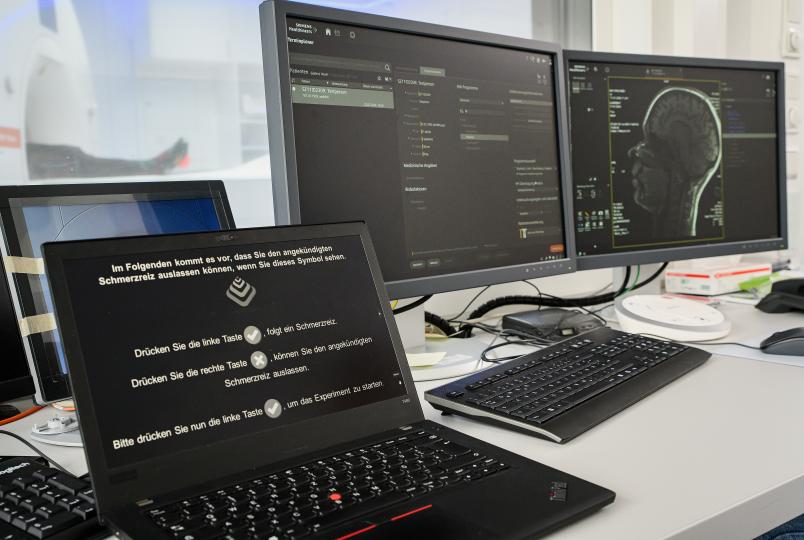
Icenhour: We have a range of experimental studies that we carry out both with patients and healthy subjects. In our conditioning studies, we often use unpleasant stimuli to produce either visceral pain, such as abdominal pain caused by pressure, or external, somatic pain, such as heat stimuli on the surface of the skin.
This is known as conditioning. Like the famous Pavlovian dog?
Icenhour: Yes, ultimately exactly the same. Incidentally, Pavlov’s dog is also an example of conditioning in the visceral domain. Whenever the dog hears a sound, it gets something to eat. At some point, the sound is sufficient for the dog to salivate. And this appetitive conditioning can be transferred to aversive learning processes. We usually work with visual stimuli, i.e. images of simple geometric shapes. A triangle, for example, is paired with a pain stimulus and can thus predict it. A circle cannot. It then serves as a safety signal.
Labrenz: We then use functional magnetic resonance imaging (fMRI) to observe what happens when the subjects see a triangle at the beginning of the experiment and what happens when they see this triangle after they have repeatedly experienced that this triangle is followed by pain. The MRI allows us to observe which brain regions become active or communicate with each other. We also work, for instance, with questionnaires and assessments. Before and after the experiment, we ask participants how they rate the stimuli on a scale from very pleasant to very unpleasant and observe learning-induced differences.
What have you observed? How is pain from the inside of the body perceived?
Icenhour: It is possible, for example, to condition participants with two different stimuli, one from the inside and one from the outside of the body, at the same time in order to make comparative statements. Prior to conditioning, our subjects rated the intensity of the two stimuli as equally strong, with the visceral stimulus being perceived as more unpleasant overall. This aversion to visceral pain increased sharply after conditioning.

The visceral stimulus was perceived as more unpleasant overall.
While the externally administered stimulus was rated as neutral, the visceral stimulus from the inside of the body was rated at over 75 on a scale from zero to 100, i.e. it was perceived as significantly more unpleasant after conditioning. A similar pattern applies to fear of pain.
Labrenz: Our subjects were able to completely ignore the external stimulus. So no significant learning process took place here. Instead, they focused more strongly on the visceral stimulus, memorized it and experienced it as much more frightening.
You keep talking about pain-related fear. So, pain memory and fear are closely intertwined?
Icenhour: Psychological factors play a central role. Many of our patients have so-called comorbidities. In addition to abdominal pain, they suffer from anxiety disorders and depression, for example. For many, fear of pain is also a major factor and prevents them from going about their daily lives.

It’s not the visceral pain that’s so bad, but the fear.
Labrenz: So it’s not the visceral pain that’s so bad, but the fear. What do I do if I get diarrhea and there is no toilet? People then stop travelling by train, switch to the car or end up staying at home altogether. Others know that they have a stressful day ahead of them and take stomach pills even though they have no symptoms.
Icenhour: So they take measures that keep the fear alive. They catastrophize, they pay increased attention to any internal signal. We want to break this vicious circle, better understand pain-related fear and, based on this, develop new forms of therapy and improve existing ones.
What could such therapies look like?
Icenhour: Psychotherapies based on the extinction of fear are also effective in chronic pain. The logical next step is now to look at the mechanisms by which these exposure therapies work in patients with chronic abdominal pain.
Labrenz: We know from anxiety research, for example, that fear avoidance behavior maintains fear and prevents extinction. We recently simulated this avoidance behavior in a pain experiment and were able to show impressively that avoidance also maintains pain-related fear.

Once we have the fear under control, then the way we deal with our pain also becomes more adaptive.
Icenhour: Similar to the treatment of anxiety disorders, you can also confront pain patients with their fear, for example by having them do specific sports exercises under supervision that involve tensing their stomach or asking them to eat foods that they have avoided for years. In this way, by confronting their fears, they learn that nothing bad will happen, or that even if they experience symptoms, they are able to manage them. Once we have the fear under control – patients feel more confident again, have positive experiences and their quality of life improves – then the way they deal with their pain also becomes more adaptive and it subsides. The subjective assessment of the pain is then different – even if it may not be completely cured.