Daniela Wenzel (left) and doctoral student Jennifer Dietrich in the laboratory
Medicine
A New Approach to Combating Asthma-induced Bronchial Remodeling
A plant-based agent inhibits a protein that, among other things, is responsible for the dreaded thickening of the bronchial wall.
Asthma medications often lose their effectiveness over time, and do not prevent the bronchial tissue from thickening. Researchers at Ruhr University Bochum, the University of Bonn, and Bonn University Hospital (Germany, have successfully tested a plant-based agent that combats this dreaded remodeling process. Derived from the coralberry Ardisia crenata, the agent inhibits a specific protein, thus ensuring that less collagen accumulates in the bronchial tissue. Less mucus is produced and secreted as well. The researchers report their findings in the journal Molecular Therapy on July 23, 2025.
Patients with bronchial asthma suffer from attacks of shortness of breath caused by constricted airways. “Anti-inflammatory medications are usually given to treat this, although it isn’t quite clear how inflammation and constriction correlate,” says Professor Daniela Wenzel, head of the Department of Systems Physiology in the Faculty of Medicine at Ruhr University Bochum. “These medications often stop working at a certain point.” Furthermore, asthma patients often experience a thickening of the bronchial tissue due to the accumulation of collagen. Goblet cells also form in increasing numbers, producing mucus and making breathing even more difficult. Currently, there is no medication to counteract these changes.
Targeting the protein directly
The agent derived from Ardisia crenata prevented the remodeling of the bronchia in the study. It binds to a specific protein – the Gq protein – and thus inhibits it directly. “Other medications often target receptors for the Gq protein, but there are many different types of receptors,” explains Jennifer Dietrich, lead author of the study. “So, we decided to take a different approach and target the protein directly.”
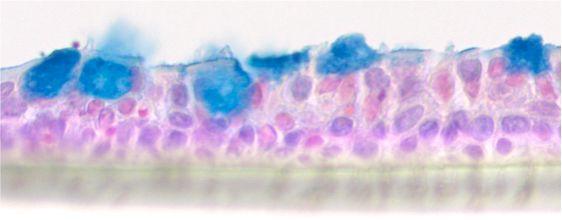
Air-liquid interface culture of human bronchial epithelial cells. Alcian blue staining shows the mucus-producing goblet cells.
Using a mouse model of chronic bronchial asthma, the researchers tested the agent for five weeks, during which it was administered directly into the lungs as a liquid. “We were able to see that the remodeling decreased, less collagen accumulated, and fewer mucus-producing goblet cells were present in the epithelial layer of the bronchial tissue,” says Dietrich. Tests on human collagen-producing cells revealed that they grew slower in the presence of the agent, even when stimulated by asthma-associated growth factors. Other tests on human mucus-producing lung cells showed that the agent reduced mucus secretion and production. These results were reproduced in experiments with lung sections from persons who had died from asthma.
A promising candidate for future treatment
“We know from past studies that the agent also prevents the extreme constriction of the bronchi,” says Daniela Wenzel. “This makes it a very promising candidate for future asthma treatments.” Once the agent binds to the Gq protein, it remains active there for several days, far longer than other agents that have been tested.